Understanding the Basics of Diabetes
Diabetic Surgery -a Treatment for Diabetes
Diabetes is a chronic metabolic disease characterized by elevated levels of blood glucose (or blood sugar); a common condition that affects people of all ages which leads over time to serious damage to the heart, blood vessels, eyes, kidneys and nerves. It develops when your pancreas does not make enough insulin hormone or any at all, or when your body is not responding to the effects of insulin.
Your blood glucose (sugar) levels are controlled by insulin, a hormone produced by pancreas. When you eat, food gets broken down into glucose which enters your bloodstream. Insulin takes the glucose out of your bloodstream and allows it to enter your cells where it is broken down and turned into energy. When glucose is in your bloodstream, it needs a “key” to reach its final destination. This key is insulin. If your pancreas is not making enough insulin or your body is not using it properly, glucose builds up in your bloodstream, causing high blood sugar (hyperglycemia).

A) Metabolic Disorder ⇄ Insulin Resistance ⇄ Type 2 Diabetes: The interconnection
There is considerable scientific evidence from studies which shows that metabolic syndrome is associated with abdominal obesity. Scientists believe obesity, especially excess fat (visceral fat) in your belly and around your organs, is a primary cause of insulin (a hormone produced by pancreas which controls blood glucose levels) resistance. Studies have shown that belly fat makes hormones and other substances that cause inflammation in your body which can lead to insulin resistance. In this case cells in your muscles, fat and liver do not respond to the insulin as the standard way they should.
Insulin helps blood glucose to enter your muscle, fat and liver cells so that it can be used as energy or stored for later use. Due to insulin resistance cells in the body can not take up the glucose in your blood efficiently which causes high blood glucose levels. In order to control the raised glucose levels the pancreas produces more insulin causing hyperinsulinemia. However, overtime insulin resistance gets worse, cells in pancreas which produce insulin get affected or damaged causing no insulin or not enough insulin production. Eventually, insulin resistance can lead to Type 2 Diabetes Mellitus. Insulin resistance is closely related to the current epidemic of diabetes. It is found in the majority of patients with type 2 diabetes, and it is present in the early prediabetic stage of impaired glucose tolerance.
The relationship between metabolic disorders, insulin resistance, and type 2 diabetes is complex and interconnected. a metabolic disorder causes insulin resistance, which in turn can lead to the development of Type 2 diabetes Mellitus,
Type2 Diabetes Mellitus is the most common type of diabetes found usually in adults, that occurs when the body becomes resistant to the insulin or fails to make insulin. In the past 3 decades the prevalence of type 2 diabetes has risen drastically in countries of all income levels. Over time, type 2 diabetes can cause serious damage to the body, especially nerves and blood vessels. Symptoms of type 2 diabetes include feeling thirsty, frequent urination, blurred vision, feeling tired and sometimes unintentional weight loss. The symptoms can be mild and may take several years to be noticed. As a result, the disease may be undiagnosed for several years after onset, when complications already arised.
B) How Metabolic Factors affect the onset of Type2 Diabetes Mellitus.:
Abnormal levels of lipids in the blood, particularly high levels of triglycerides and low levels of HDL (Good Cholesterol), are associated with an increased risk of Type2 Diabetes Mellitus. Dyslipidemia is often seen in conjunction with obesity and insulin resistance.
Reduced β-Cell Sensitivity: β-Cells are responsible for insulin production, when the β-cells reduce sensitivity or act abnormally that can lead to inadequate production of insulin in response to blood glucose levels, promoting the onset of diabetes.
Hyperinsulinemia: Initially, the body compensates for insulin resistance by producing more insulin, leading to hyperinsulinemia. Over time, this can exhaust the β-cells, leading to their dysfunction and eventual onset of Type2 Diabetes Mellitus.
Glucagon is a hormone that raises blood glucose levels to sustain blood glucose homeostasis in the body by promoting the release of glucose from the liver by the process Glycogenolysis. In insulin resistance, glucagon activity is often disturbed, leading to elevated blood glucose levels (hyperglycemia), especially in the fasting state.
Over time, uncontrolled diabetes can damage blood vessels in the heart, eyes, kidneys and nerves. Diabetes can cause permanent vision loss by damaging blood vessels in the eyes. People with diabetes have a greater risk of developing health conditions like heart attack, stroke and kidney failures. Many patients develop problems with their feet causing nerve damage, foot ulcers and may lead to amputation
Understanding the Metabolic conditions, its risk factors and complications becomes crucial in order to prevent and treat severe life threatening health conditions like Type2 diabetes and its related disease, stroke and organ damage. The effective management helps improve the symptoms of disease, reduce the risk, slows down the progression of disease and controls the emergency situations. Additionally treatment improves and resolves the health condition, leading to high quality life.
C) The Prevention and Treatment strategy includes:
I) Prevention Strategies -
Healthy Lifestyle: Engage in regular physical activity, maintain a healthy diet, avoid smoking, and limit alcohol consumption.
Weight Management: Maintain a healthy weight to reduce the burden on insulin production and function.
Regular Screening: Monitor blood glucose, lipid levels, and other metabolic markers regularly, especially if you have a family history of diabetes or other risk factors.
II) Treatment Strategies -
Medical Intervention: In some cases, medications may be necessary to manage blood glucose levels, lipid levels, and other related conditions.
Surgical Interventions: A Metabolic; a Bariatric Surgery to treat obesity, a root cause for Type2 diabetes which can help to induce significant weight loss and improve metabolic outcomes.
D) What is Metabolic; a Diabetic Surgery? Understanding the mechanism behind Diabetes Management & Weight loss.
Metabolic surgery; a Diabetic surgery is a gastrointestinal surgery primarily used to treat obesity and related conditions such as Type 2 Diabetes (T2D). It provides the most substantial and sustainable weight loss in individuals with obesity. The highly effective solution to treat Type2 Diabetes, which often promotes significant improvements in other obesity related conditions such as hypertension, sleep apnea, and joint problems etc. The main mechanism behind these surgeries lies in reducing the size of the stomach, altering digestion, and influencing the hormonal pathways that regulate metabolism, appetite, and blood sugar control.
The surgery can be done laparoscopically which include Sleeve Gastrectomy (SG), One Anastomosis Gastric Bypass- OAGB, Roux-en-Y gastric Bypass (RYGB), as follows.
Laparoscopic Sleeve Gastrectomy: Laparoscopic Sleeve Gastrectomy is the most commonly performed weight loss surgery world-wide. This is a minimally invasive weight-loss surgery that involves removing a significant portion of the stomach to reduce its size and limit food intake. By making small incisions and using a laparoscope (a thin, long tube with a camera), the surgeon can perform the procedure with greater precision without a risk.
Mechanism:
The reduced stomach size limits the food intake, this can help patients feel full more quickly, which can lead to eating less.
Alterations in gut hormones affect hunger and satiety signals (e.g., reduced ghrelin, the hunger hormone).
These anatomic changes also lead to alterations in the signaling between luminal factors and the intestinal mucosa, thus generating neurohumoral effects that lead to alterations in hunger, satiety, regulating hormones, and weight loss.
One Anastomosis Gastric Bypass- OAGB Surgery
The OAGB surgery is initiated by reducing the size of the stomach so that it requires less food. The stomach is converted into a long slender pouch up to the antral part by stapling. The second step of the surgery involves the creation of a bypass for food to flow from the new stomach pouch. A loop of the small intestine is chosen depending upon the surgeon and the metabolic condition of the patient.
The middle section of intestine is attached to the opening in the stomach pouch creating what is referred to as the “omega loop”. The loop enables food to bypass the lower stomach, duodenum, and a portion of the small intestine. At the end of the procedure, the incisions are closed with sutures.
There is evidence from different studies which says patients with morbid obesity after OAGB show a significant decrease in BMI and fasting blood glucose concentration. It shows an improved lipid profile and decreased levels of triglycerides which is beneficial for improving glucose sensitivity and cardiovascular health.
Mechanism:
The reduced stomach size limits the food intake, this can help patients feel full more quickly, which can lead to eating less.
It decreases the production of hormones that increase appetite.
Rerouting the gastrointestinal tract causes the body to respond quickly by changing hormone levels, which can mimic insulin and improve metabolic response.
OAGB, being a restrictive and malabsorptive procedure, limits the intake and absorption of fat which results in burning the stored fat in the body for the energy purpose thus promoting weight loss.
Gastric Bypass Surgery: is also known as ‘The Roux-en-Y gastric bypass’ that involves creating a small pouch by dividing the top of the stomach from the rest of the stomach. Then small intestine is divided, and the bottom end of the divided small intestine is connected to the newly created small stomach pouch and in the end, the top portion of the divided small intestine is connected to the small intestine further down so that the stomach acids and digestive enzymes from the bypassed stomach and first portion of your small intestine will eventually mix with the food.
Mechanism:
These anatomic changes reduce the amount of food intake and one can feel full faster, as a result, you consume and absorb less calories.
The surgery can also change hormones in the gastrointestinal tract that further lead to alterations in hunger, satiety, energy balance, and weight loss.
Bypassing a portion of the intestine enhances glucose control by improving insulin action.
These procedures work by physically reducing stomach size and creating significant hormonal changes that improve metabolic health and can lead to remission of Type 2 Diabetes. Thus the procedure can help stabilize metabolism and regulate blood sugar.
However, taking proper care after bariatric surgery is essential for ensuring a successful recovery and achieving long-term weight-loss goals. The dietary guidelines, staying hydrated, taking necessary supplements, and gradually incorporating exercise are critical components of post-surgery care. Regular follow-up appointments with your healthcare team and monitoring for any symptoms, will further contribute to your overall well-being.
E) Eligibility Criteria for Undergoing Metabolic/Diabetic surgery:
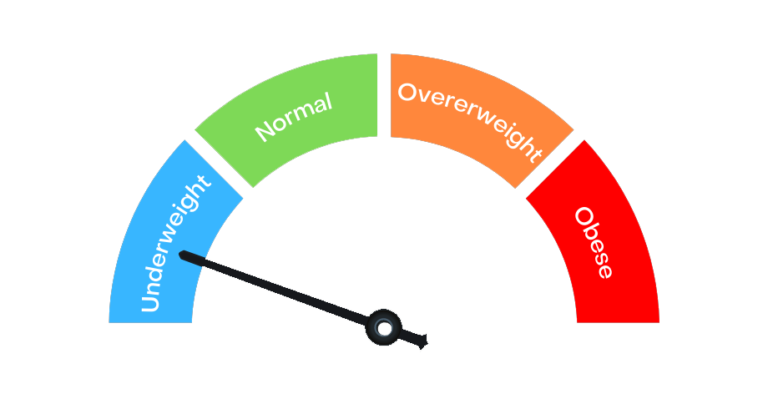
When determining a candidate’s eligibility for metabolic surgeries, several factors should be considered such as BMI, obesity related health conditions, should be motivated to lose weight etc. Meeting the criteria for bariatric surgery is crucial not only for the successful and sustained weight loss but also for the long-term health and well-being of the patient.
Body Mass Index: The numerous randomized clinical trials demonstrate that metabolic surgery achieves excellent glycemic control and reduces cardiovascular risk factors. On the basis of such evidence and recent clinical guidelines, metabolic surgery should be recommended in patients with BMI ≥ 30.0 kg/m2 and BMI more than 27.0 kg/m2 if patient is having hyperglycemia that is inadequately controlled despite optimal treatment with either oral or injectable medications.
Obesity-Related Health Conditions Assessment: The presence of obesity related health conditions such as type 2 diabetes, hypertension, high cholesterol, sleep apnea, or joint problems, PCOS, Infertility, etc. can influence eligibility. All these metabolic conditions may indicate a greater need for weight-loss surgery.
Failed previous weight loss attempt: Doctors look at the patient’s history of previous weight loss attempts through diet, exercise, and medications. Typically, surgery is considered when non-surgical methods have been unsuccessful.
Overall, Health: Medical Evaluation is necessary to determine if the patient is fit for surgery. This includes evaluating heart health, lung function, liver health, and any other underlying medical conditions.
Medication if any: Before undergoing Bariatric surgery, the doctor will check the medications that patient might be taking and will recommend reducing them or stopping them if required.
Psychological Evaluation: It becomes necessary to assess the psychological condition of a patient to identify any issues like depression or anxiety, to know the patient’s mental readiness for bariatric surgery to understand behavioral pattern; emotional overeating and need for counseling.
Age: The age of a patient should be between 14 -70 years, the exact age criteria can vary depending on the specific procedure and the individual’s health conditions and also other criteria which are to be met.
Unhealthy habits: A person should not have any unhealthy habit like smoking and alcohol before surgery and after surgery as Bariatric Surgery requires to have a healthy lifestyle.
F) Minimized Complications associated with the surgeries:
There is still a lack of awareness about metabolic diseases like Type2 Diabetes, its related medical health issues and modern treatment options available to manage or even reverse them. People are still afraid of metabolic surgery and its complications. Unlike any other surgery it has negligible complications like leaks, bleeding infection. With advanced technologies, techniques, expertise, experience and post operated care the complications associated with the procedures have significantly minimized as follows:
Leaks: unlike the traditional surgical method, with the improved techniques, technology, and the better surgical materials the risk of leaking has minimized considerably.
Bleeding: Any surgery has a risk of bleeding, but the modern metabolic/ Bariatric surgeries are performed more precisely, significantly minimizing the risk of bleeding.
Infections: Advanced sterile surgical practices and post-operative care have drastically minimized the risk of infections.
It is very crucial to understand the importance of the metabolic/ Bariatric surgeries which not only reduces your weight but beyond that it improves your overall health and lifestyle.
G) Benefits of Metabolic surgery: A Treatment for Diabetic.
The surgery helps resolve obesity and its related conditions like Type2 Diabetes. It can significantly improve or resolve obesity-related conditions like Type2 Diabetes. There is high quality evidence which has supported metabolic surgery as an effective means of treating Type2 Diabetes Mellitus. The procedure improves glucose metabolic profiles by reducing glycated hemoglobin (HbAlc) and at the same time increasing circulating incretin concentrations, insulin sensitivity and b-cell function. Many patients with Type2 Diabetes who undergo these procedures have experienced complete remission of the diabetes, who are having normal HbAlc fasting blood glucose without need of antidiabetic drugs.
Effective and sustained weight loss: Metabolic surgeries like Sleeve Gastrectomy, OAGB surgery and the Roux-en-Y gastric bypass (RYGB) results in effective and sustained weight loss which is not possible with non surgical weight loss methods.
Caloric Restriction: Shortening or bypassing the small intestine and reducing the size of the stomach results in decreased food and calorie intake. Calorie restriction helps directly in weight loss. This is a key factor in improving metabolic health.
Increased nutrient delivery to the distal small intestine: In some surgeries like One Anastomosis Gastric Bypass-OAGB the digestive tract is rerouted by bypassing a portion of the small intestine, allowing the nutrient to reach directly to the lower part of the small intestine more quickly. Thus rapid delivery of nutrients triggers the release of hormones that enhances the insulin sensitivity, promotes satiety which helps in weight loss and better glucose control.
Changing digestive hormones: Metabolic surgeries/Bariatric surgery can also alter digestive hormones, which can reduce hunger signals that travel from the digestive system to the brain.
There is some ongoing research on Gut hormone profiles after Bariatric surgery which clarifies the complex role of hormones in eating behavior, weight loss and improved metabolic health. There is evidence of change in appetite within a day after Bariatric surgery.
A recent study has further demonstrated that postprandial PYY and GLP-1 profiles start rising as early as 2 days following the operation which helps in reducing appetite.
Bariatric surgery, especially sleeve gastrectomy reduces the production of ghrelin leading to reduced hunger and calorie intake.
It can lead to changes in leptin levels and its signaling pathways, contributing to further weight loss and reduced appetite.
It also improves insulin sensitivity leading to improved glucose metabolism. It positively impacts metabolic health by altering the levels of various adipokines.
Changes in the Gut Microbiome: The gut microbiome, which is the collection of microorganisms living in the digestive tract, undergoes significant changes after surgery. These changes can enhance metabolism, improve glucose control, and reduce inflammation, further supporting weight loss and metabolic health.
These physiological changes not only lead to weight loss but result in favorable hormonal shifts that improve glucose metabolism. The improved glucose control and reduced insulin resistance contribute to a lower risk of Type2 Diabetes, cardiovascular events, such as heart attacks and strokes, and overall mortality. Thus, Bariatric surgery can be a transformative treatment option which leads to significant improvements in quality of life and long-term health outcomes.
Conclusion
Several studies have highlighted the remarkable benefits of Metabolic/ Bariatric surgery, not only in weight loss but also in treating Type 2 Diabetes Mellitus (T2DM). These surgeries address the root causes of metabolic disorders and significantly improve glycemic control and insulin sensitivity.
Beyond just weight loss the metabolic surgery treats Type2 Diabetes by enhancing the glucose metabolism, It improves other obesity and Type2 Diabetes related health conditions thus improves overall metabolic health. With the advanced surgical techniques the complications related to surgery have been minimized, making these procedures more safe and beneficial for the patients.
In a world where obesity and diabetes are on the rise, metabolic surgery offers a promising solution for long-term health improvement. As a result, they are an effective treatment for managing and potentially reversing T2DM and related conditions.

Dt. Kshama Bhoir
Bariatric Dietician & Content Writer