Dt. Amisha
Bariatric Dietician & Content Writer
Impact of Bariatric Surgery on Metabolic Disorders
Bariatric surgery, a set of surgical procedures aimed at reducing obesity, has been shown to have significant effects on metabolic disorders, often resulting in their improvement or resolution. Some of the key metabolic disorders affected by bariatric surgery include:
Type 2 Diabetes Mellitus (T2DM): Bariatric surgery has been found in reversal of T2DM in a significant proportion of patients. This remission can occur rapidly, sometimes even before significant weight loss is observed, suggesting that mechanisms beyond weight reduction may be at play. Bariatric procedures such as Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy have been particularly effective in improving glucose metabolism and insulin sensitivity.
Ways in which bariatric surgery helps in reducing DM –
Bariatric surgery helps in Type 2 Diabetes Mellitus (T2DM) by making significant changes in how the body processes glucose, leading to improved blood sugar control. In simple terms, here’s how it works:
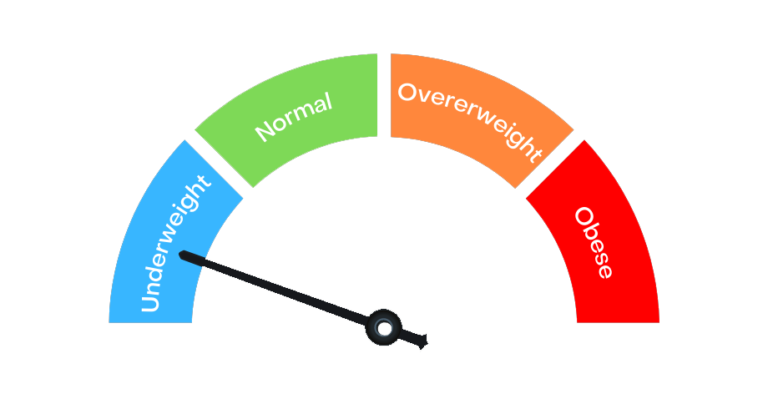
When someone has T2DM, their body struggles to regulate blood sugar levels properly. This can happen because of excess weight and fat, which can make cells resistant to insulin, the hormone responsible for moving sugar from the blood into cells to be used for energy. Bariatric surgery addresses this in a few ways.
Firstly, it leads to significant weight loss, reducing the burden on the body’s insulin-producing cells in the pancreas. Secondly, it alters the gut hormones involved in appetite and metabolism, leading to improved insulin sensitivity and better blood sugar control. Lastly, changes in the digestive tract after surgery can affect how nutrients are absorbed, further helping regulate blood sugar levels.
These combined effects often result in rapid improvements in T2DM symptoms and, in many cases, even remission of the disease. Some people may no longer need diabetes medication or insulin after bariatric surgery.
At Aastha Bariatrics, the majority of patients have experienced such significant improvements in their diabetes that they no longer need to take medications or insulin. Many patients who originally had HbA1c levels as high as 11-12% before surgery have seen their levels drop to a much healthier range of 5-7% after the procedure.
Hypertension (High Blood Pressure): Bariatric surgery often leads to significant reductions in blood pressure, with many patients experiencing normalization of blood pressure levels. This improvement in hypertension is thought to be related to weight loss, changes in hormonal regulation, and alterations in the renin-angiotensin-aldosterone system.
Testimonials at Aastha Bariatrics, have successfully reversed their hypertension to the extent that they no longer require medications. Patients who initially presented with high blood pressure readings, for example, systolic blood pressure readings of 160-180 mmHg and diastolic readings of 100-110 mmHg, have seen remarkable improvements post-surgery.
After undergoing bariatric procedures, their blood pressure readings have dropped to a much healthier range, typically between 110-130 mmHg systolic and 70-80 mmHg diastolic. This improvement is akin to a significant reduction in hypertension severity from severe or stage 2 hypertension to mild or moderate hypertension, or even within the normal range for some patients. Consequently, many patients have been able to discontinue their hypertension medications altogether.
Dyslipidemia (Abnormal Blood Lipid Levels): Bariatric surgery typically results in favorable changes in lipid profiles, including reductions in total cholesterol, low-density lipoprotein (LDL) cholesterol, and triglycerides, as well as increases in high-density lipoprotein (HDL) cholesterol. These changes contribute to a lower risk of cardiovascular disease.
Non-alcoholic Fatty Liver Disease (NAFLD): Bariatric surgery has been shown to improve liver histology and reduce liver fat content in patients with NAFLD, leading to a decrease in inflammation and fibrosis. This improvement in liver health is often observed alongside weight loss and improvements in metabolic parameters.
Obstructive Sleep Apnea (OSA): Bariatric surgery can lead to significant improvements in OSA, including reductions in the severity of apnea-hypopnea episodes and improvements in daytime symptoms such as excessive daytime sleepiness.
These improvements are thought to result from weight loss, reduction in visceral fat, and changes in upper airway anatomy. Approximately 80% of patients seeking treatment at AASTHA HOSPITAL suffer from sleep apnea, indicating that obesity serves as a predominant factor contributing to this condition.
At Aastha Bariatrics, many patients have experienced significant improvement in their sleep apnea following bariatric surgery. Patients who previously struggled with severe sleep apnea, characterized by frequent episodes of breathing pauses during sleep, have seen remarkable changes post-surgery.
Furthermore, patients who previously experienced daytime fatigue, snoring, and other symptoms of sleep apnea have reported resolution or substantial alleviation of these issues post-surgery.
Polycystic Ovary Syndrome (PCOS): Bariatric surgery has been shown to improve symptoms and metabolic parameters in women with PCOS, including menstrual regularity, insulin resistance, and androgen levels. These improvements can enhance fertility and reduce the long-term risk of complications associated with PCOS.